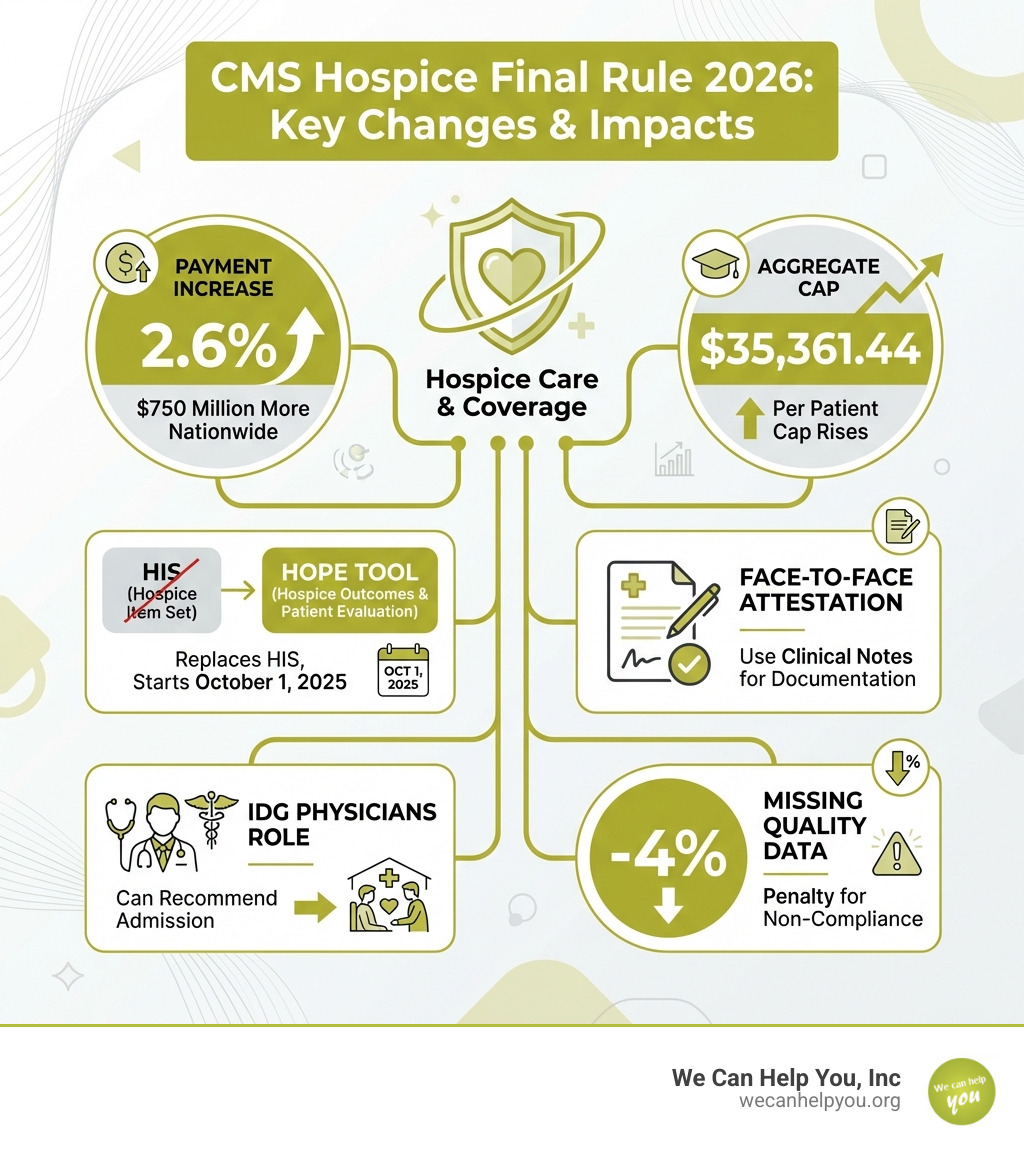
Why the CMS Hospice Final Rule 2026 Matters for Your Care and Coverage
The cms hospice final rule 2026 brings significant changes to Medicare hospice payments, quality reporting, and operational requirements that take effect October 1, 2025. Whether you’re a family member supporting a loved one in hospice or planning ahead for your own care, understanding these updates helps you know what to expect from hospice providers.
Key changes at a glance:
- Payment increase: 2.6% overall update, adding approximately $750 million nationwide
- New aggregate cap: $35,361.44 per patient (up from $34,465.34)
- Quality reporting shift: Mandatory transition from HIS to the HOPE tool
- Attestation flexibility: Physicians can now use clinical notes for face-to-face encounter documentation
- Expanded physician roles: IDG physicians can recommend hospice admission
- Penalty for non-compliance: Hospices failing to submit required quality data face a -1.4% payment reduction instead of the increase
On August 1, 2025, the Centers for Medicare & Medicaid Services (CMS) issued this final rule (CMS-1835-F) to update how Medicare pays hospice providers and what quality standards they must meet. The changes affect everything from daily care rates to how hospices document patient encounters.
For families navigating end-of-life care decisions, these changes mean hospice providers will have updated resources and clearer guidelines. The payment adjustments help hospices maintain staff and services despite rising costs, while the new HOPE tool aims to improve how providers track and report patient outcomes.
The rule also addresses practical concerns. For example, the new flexibility around attestation requirements means less paperwork burden on physicians while maintaining quality oversight. The wage index adjustments account for geographic cost differences, so hospices in higher-cost areas receive appropriate payment levels.
Understanding these changes matters because hospice care is often a critical part of Medicare coverage during life’s final chapter. The estimated $750 million increase in payments reflects the government’s recognition that hospice providers face real cost pressures while delivering compassionate, person-centered care.
The Bottom Line: FY 2026 Hospice Payment Updates
The Centers for Medicare & Medicaid Services (CMS) has finalized a 2.6% payment update for Fiscal Year (FY) 2026, which begins on October 1, 2025. This update is a crucial element of the cms hospice final rule 2026 and reflects ongoing efforts to ensure fair compensation for hospice services.
This 2.6% payment update is based on a 3.3% inpatient hospital market basket percentage increase, reduced by a 0.7 percentage point productivity adjustment. While this finalized percentage is higher than what was initially proposed, it still represents an estimated increase of $750 million in payments from FY 2025 across the nation. However, some industry advocates, such as the National Alliance for Care at Home, have voiced concerns that this increase might still not be enough to fully offset the persistent inflationary pressures and the ongoing healthcare workforce crisis faced by hospice providers in our communities, from California to New York.
Another significant update is the new aggregate cap amount for hospice payments. For FY 2026, this cap has been set at $35,361.44 per patient. This is an increase from the FY 2025 cap of $34,465.34. The aggregate cap serves as a limit on the total Medicare payments a hospice can receive in an accounting year, ensuring fiscal responsibility within the program.
It’s also vital for hospices to be aware of the financial implications of failing to meet quality data submission requirements. If a hospice does not submit the required quality data, they will face a substantial 4 percentage point reduction in their annual payment update. For FY 2026, this means that instead of receiving the 2.6% increase, non-compliant hospices would experience a -1.4% reduction over the previous year’s payment rate. This penalty underscores the importance of stringent quality reporting for all hospices, including those serving patients in places like Florida, Ohio, and Texas.
The rule also includes a technical but impactful change related to how payments are calculated. The inpatient hospital market basket, which is used to determine hospice payment rate updates, will be rebased and revised to a 2023 base year for FY 2026. This adjustment helps ensure that the payment rates accurately reflect the current costs of goods and services used by hospitals, which then informs the reimbursement rates for hospices.
For a deeper dive into how these changes might affect your personal Medicare costs, you can find more info about Medicare costs.
New Payment Rates by Level of Care
Understanding the specific payment rates for different levels of hospice care is crucial for both providers and beneficiaries. These rates are adjusted annually and reflect the resources required for each type of service. For FY 2026, the finalized payment rates are:
- Routine Home Care (RHC) Days 1–60: $230.83 per day
- Routine Home Care (RHC) Days 61+: $181.94 per day
- Continuous Home Care (CHC): $1,674.29 per day (equating to $69.76 per hour)
- Inpatient Respite Care (IRC): $532.48 per day
- General Inpatient Care (GIP): $1,199.86 per day
These rates are then further adjusted based on the hospice wage index applicable to the specific geographic area where the services are provided.
Understanding the Hospice Wage Index Adjustments
The hospice wage index plays a critical role in ensuring that Medicare payments account for the varying costs of labor across different regions. This index adjusts payment rates for geographic wage differences, reflecting that it costs more to provide care in a high-wage area like Newark, New Jersey, compared to a lower-wage area.
For FY 2026, the hospice wage index is based on the current fiscal year’s hospital pre-floor, pre-reclassified hospital wage index data. This methodology aims to ensure that hospice payments accurately reflect local labor market conditions.
CMS has also maintained a permanent 5% cap on any decrease to a geographic area’s wage index from its prior year’s wage index. This policy provides a safeguard against sharp, sudden reductions in payments due to wage index fluctuations, offering stability for hospices in states like Georgia and Ohio. For FY 2026, this 5% cap on wage index decreases will continue to be applied at the county level.
The wage index also incorporates the Office of Management and Budget (OMB) statistical area delineations. These delineations, based on the most recent Decennial Census, define metropolitan and micropolitan statistical areas. Changes in these delineations can lead to counties being reclassified from urban to rural or vice versa, directly impacting the wage index applied to hospices in those areas. For example, specific counties in states like Florida or California might see adjustments based on these reclassifications.
Finally, CMS has revised the labor shares for wage-adjusting hospice payments for each level of care. These percentages determine how much of the payment rate is subject to the wage index adjustment: 66% for Routine Home Care, 75.2% for Continuous Home Care, 61% for Inpatient Respite Care, and 63.5% for General Inpatient Care.
You can find the final hospice wage index for FY 2026 directly on the CMS website.
Major Quality Reporting and Operational Shifts in the cms hospice final rule 2026
The cms hospice final rule 2026 isn’t just about payment rates; it also introduces significant changes to how hospices report quality data and manage certain operational aspects. These updates are designed to improve accountability, streamline processes, and ultimately improve the quality of care for patients and families.

At the heart of these changes is the Hospice Quality Reporting Program (HQRP), which requires hospices to submit specific data to CMS. This program is evolving, with the most shift being the transition from the familiar Hospice Item Set (HIS) to the new Hospice Outcomes & Patient Evaluation (HOPE) tool. These data submissions are critical for hospices to avoid payment penalties and demonstrate their commitment to high-quality care.
The Transition from HIS to the HOPE Tool
The biggest news in quality reporting for the cms hospice final rule 2026 is the mandatory transition from the Hospice Item Set (HIS) to the Hospice Outcomes & Patient Evaluation (HOPE) tool. This is a monumental shift that all hospices, including those in our service areas like New Jersey, Ohio, and Georgia, must prepare for.
The full implementation of the HOPE tool is scheduled for October 1, 2025. From this date forward, HIS will no longer be accepted for admissions and discharges. Furthermore, the QIES system will stop accepting HIS records for events that occurred prior to October 1, 2025, on February 15, 2026. This means there’s a hard deadline for wrapping up all HIS-related submissions.
All HOPE data submissions will be made through the iQIES (Internet Quality Improvement and Evaluation System) platform. Providers must ensure they have access to this system and that their staff are thoroughly trained on its use.
While the data collection begins in FY 2026, public reporting of HOPE-based quality measures is anticipated to begin no earlier than FY 2028 (specifically, no earlier than November 2027). This public reporting will be based on data collected from four quarters of Calendar Year 2026.
To avoid payment penalties, hospices must meet a strict data submission threshold: 90% of all required HIS/HOPE records must be submitted within 30 days of the patient event. This timely submission requirement applies to the HOPE tool once it’s implemented.
It’s also important to note who can complete the HOPE assessment. An RN is required for the clinical assessment items within HOPE, while LPN/LVNs may complete Symptom Follow-up Visits (SFVs). Other qualified staff can handle administrative data. Symptom Follow-up Visits may be required for patients based on certain symptom severity scores, with up to three potentially needed per stay.
For the latest updates and resources related to HOPE data submission specifications, you can always find the latest HOPE technical information directly from CMS. For more general information about hospice care, we encourage you to learn more about hospice care.
Key Changes to Physician Roles and Patient Attestation
The cms hospice final rule 2026 also brings welcome clarifications and flexibility regarding physician roles and patient attestation requirements, aiming to reduce administrative burden while maintaining oversight.
Firstly, CMS has clarified that a physician member of the hospice interdisciplinary group (IDG) can now recommend admission to hospice care. This is a significant alignment of regulations with existing certification and Conditions of Participation (CoPs) requirements. It acknowledges the comprehensive role of the IDG in patient assessment and care planning, potentially streamlining the initial steps of the admission process. While an IDG physician can recommend, the final certification of terminal illness still needs to be completed by the hospice medical director or a designated physician. You can read the regulation on hospice admission for the precise wording.
Secondly, the rule introduces greater flexibility for the face-to-face encounter attestation requirements. Previously, there was often confusion or a need for separate forms. Now, while the attestation must still include the physician’s or nurse practitioner’s signature and date, it can be satisfied by a signed and dated clinical note within the medical record. This means that as long as the clinical note clearly indicates that the face-to-face encounter occurred and includes the necessary details, a separate attestation form is no longer strictly required. This change aims to reduce administrative burden on busy clinicians, a welcome relief for providers in our communities from California to Florida.
Lastly, it’s worth noting that telehealth can continue to be used for hospice recertification face-to-face encounters until September 30, 2025.
Preparing Your Agency: Key Takeaways and Action Steps
With the cms hospice final rule 2026 just around the corner, preparation is paramount for hospice providers. Navigating these changes effectively means focusing on financial adjustments, policy updates, and staff readiness.
Hospices must conduct a thorough review of the financial impact of these changes. This includes analyzing the new payment rates and understanding how the wage index adjustments will specifically affect their operations in their respective Core Based Statistical Areas (CBSAs). For a hospice in Albany, Georgia, the impact might be different from one in Toledo, Ohio, or Newark, New Jersey, where we’ve seen various changes in Routine Home Care rates.
Budget adjustments will be necessary to account for the new payment rates and any changes resulting from the wage index. This financial foresight is critical for maintaining stability and ensuring continued high-quality care.
Internal policies and procedures will need updating to align with the new physician roles and the expanded flexibility in face-to-face attestation. Ensuring that all staff are aware of these changes and how they impact daily operations is key to smooth implementation.
Perhaps most importantly, comprehensive staff training on the new HOPE tool and the iQIES platform is essential. This includes training for clinical staff on data collection, as well as administrative staff on submission processes.
Finally, regular compliance audits of data submission processes will be crucial to ensure that HQRP requirements are consistently met. This proactive approach helps hospices avoid the steep payment penalties associated with non-compliance.
For more information and resources on these regulatory changes, visit the Center for Medicare Services website.
Your Agency’s Checklist for the cms hospice final rule 2026
To help your hospice agency confidently steer the upcoming changes, we’ve put together a concise checklist of actionable steps:
- Review your CBSA-specific wage index to project the precise financial impact of the new rates on your agency’s budget.
- Update all billing systems with the new FY 2026 payment rates well before October 1, 2025, to ensure accurate claims processing.
- Train all clinical staff extensively on the HOPE tool’s data collection requirements and the iQIES platform for submission.
- Revise internal policies and documentation procedures for face-to-face attestation to include the flexibility of using signed and dated clinical notes.
- Ensure all staff, especially interdisciplinary group members, understand the IDG physician’s expanded role in recommending hospice admission.
- Implement or improve ongoing compliance audits for your quality data submission processes to consistently meet the 90% HQRP threshold and avoid payment penalties.
Frequently Asked Questions about the CMS Hospice Final Rule
We understand that navigating these regulatory changes can bring up many questions. Here are some of the most common ones we’ve encountered regarding the cms hospice final rule 2026:
What is the biggest change in the FY 2026 rule?
The most significant change is the mandatory transition from the Hospice Item Set (HIS) to the new Hospice Outcomes & Patient Evaluation (HOPE) tool for all quality reporting, effective October 1, 2025. This requires new training, software integration, and data submission processes via the iQIES platform. This shift aims to standardize data collection and improve the consistency and quality of reported patient outcomes.
What happens if my hospice fails to meet quality reporting requirements?
Hospices that fail to submit the required quality data (at least 90% of all required HOPE records within 30 days of the patient event) will face a 4-percentage point reduction in their annual payment update. For FY 2026, this means that the 2.6% payment increase would turn into a -1.4% payment reduction, a significant financial consequence for non-compliance.
Can any physician in the interdisciplinary group (IDG) now certify a patient for hospice?
The rule clarifies that a physician member of the IDG can recommend a patient for hospice admission, aligning with existing certification and Conditions of Participation (CoPs) regulations. This streamlines the initial assessment process. However, it’s important to note that this does not change the final certification requirement, which must still be completed by the hospice medical director or a designated physician.
Conclusion
The cms hospice final rule 2026 brings a mix of payment increases, crucial quality reporting transitions, and operational clarifications that will shape hospice care delivery in the coming fiscal year. With a 2.6% payment increase, a new aggregate cap, and the mandatory shift to the HOPE tool, hospice providers have much to digest and implement by October 1, 2025.
These changes highlight CMS’s ongoing commitment to refining the Medicare hospice benefit, ensuring sustainable payments, and improving the quality of end-of-life care. For hospices, diligent preparation is key to navigating these operational shifts and maintaining financial stability.
Navigating these CMS changes is crucial for providing quality care. We Can Help You, Inc. is dedicated to helping individuals understand their Medicare benefits, including hospice coverage. For a comprehensive overview of hospice coverage, explore our guide on navigating Medicare and hospice care.



